Ventilator Modes, Initial Settings, and Patient-Ventilator Asynchrony
Mechanical ventilation is a fundamental aspect of critical care, essential for managing respiratory failure. This guide provides an in-depth explanation covering ventilator modes, initial settings, asynchrony, and lung-protective strategies, structured for postgraduate exams, including theory, viva, and MCQs.
I. Ventilator Modes
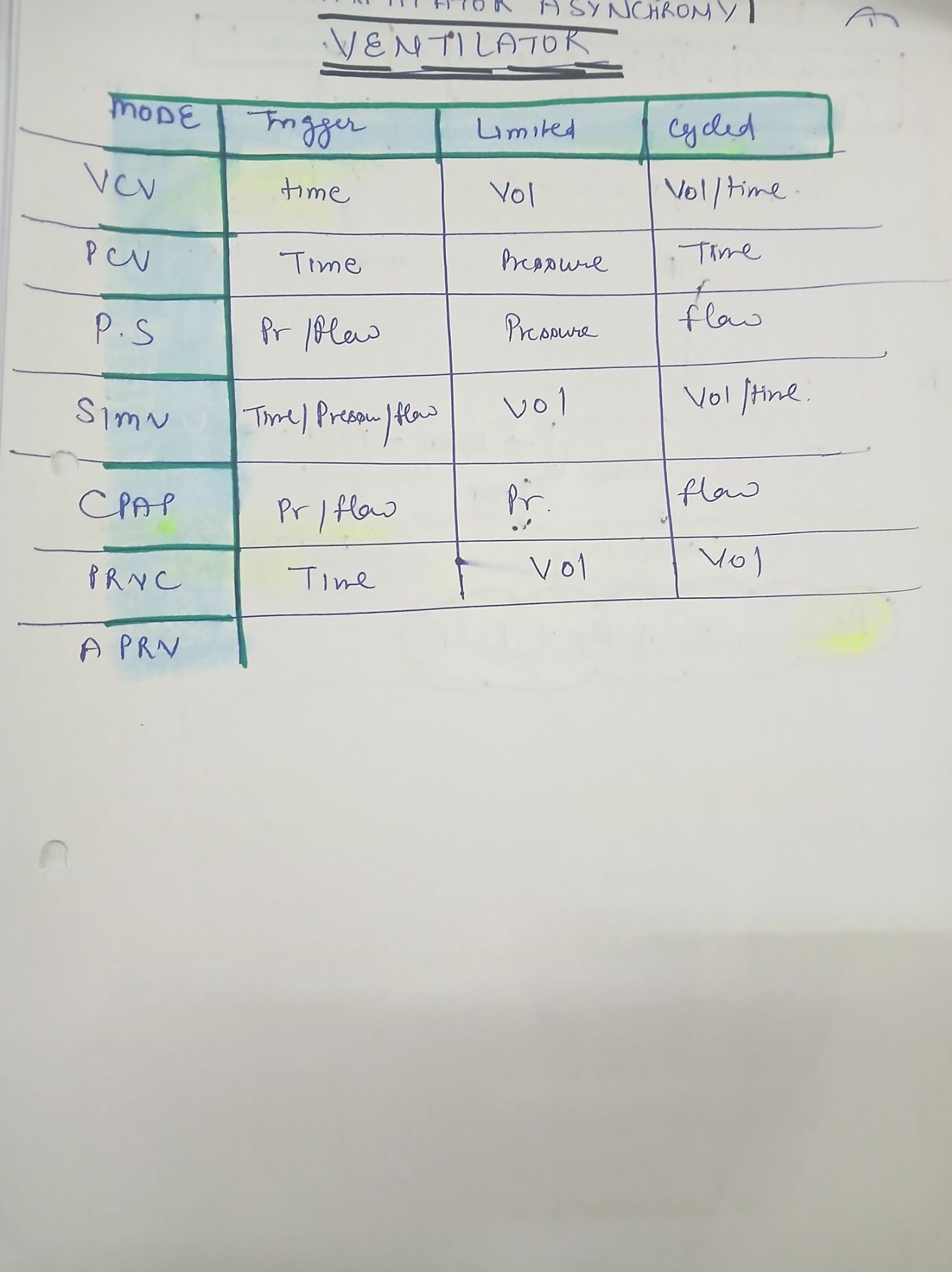
Ventilator modes are classified based on:
• Trigger: The mechanism initiating a breath (time- or patient-triggered).
• Limit: The parameter controlled during inspiration (pressure or volume).
• Cycle: What terminates inspiration (time, volume, flow, or pressure).
- Control Variable: The main variable controlled by the ventilator (pressure or volume).
A. Volume-Controlled Modes (VCV)
• Trigger: Time-triggered (mandatory) or patient-triggered (assisted).
• Limit: Flow-limited (constant or decelerating flow).
• Cycle: Volume-cycled (breath ends when a preset tidal volume is delivered).
• Control Variable: Volume.
• Use: Ensures consistent minute ventilation, ideal for post-op patients and neuromuscular disorders.
• Disadvantage: High peak inspiratory pressure (PIP) in conditions like ARDS.
1. Volume-Controlled Continuous Mandatory Ventilation (VC-CMV)
• All breaths are machine-controlled (time- or patient-triggered).
• No spontaneous breathing without ventilator assistance.
• Indications: Deep sedation, neuromuscular blockade.
• Risk: Ventilator asynchrony if the patient attempts spontaneous efforts.
2. Volume-Controlled Synchronized Intermittent Mandatory Ventilation (VC-SIMV)
• Provides a set number of mandatory breaths but allows spontaneous breathing between them.
• Indications: Weaning, post-operative management.
• Advantage: Reduces ventilator dependence compared to CMV.
B. Pressure-Controlled Modes (PCV)
• Trigger: Time- or patient-triggered.
• Limit: Pressure-limited.
• Cycle: Time-cycled (preset inspiratory time).
• Control Variable: Pressure.
• Use: ARDS, lung-protective ventilation.
• Disadvantage: Tidal volume varies with lung compliance.
1. Pressure-Controlled Continuous Mandatory Ventilation (PC-CMV)
• All breaths are mandatory and pressure-limited.
• Ensures lower peak airway pressures but variable tidal volumes.
• Indications: ARDS, lung-protective strategies.
2. Pressure Support Ventilation (PSV)
• Trigger: Patient-triggered.
• Limit: Pressure-limited (preset pressure support).
• Cycle: Flow-cycled (breath ends when inspiratory flow decreases).
• Use: Weaning and promoting spontaneous breathing.
• Advantage: Better synchrony, reduced work of breathing.
C. Hybrid and Advanced Modes
• Adaptive Support Ventilation (ASV): Adjusts tidal volume and respiratory rate dynamically.
• Proportional Assist Ventilation (PAV): Proportional assistance based on patient effort.
• Neurally Adjusted Ventilatory Assist (NAVA): Uses diaphragmatic electrical activity to control ventilator support.
II. Initial Ventilator Settings
|
Parameter |
Normal Lungs |
ARDS |
COPD/Asthma |
|
Tidal Volume (VT) |
6-8 mL/kg IBW |
4-6 mL/kg IBW |
6-8 mL/kg IBW |
|
Respiratory Rate (RR) |
12-16/min |
18-25/min |
8-12/min |
|
FiO₂ |
100% → Wean to SpO₂ 92-96% |
100% → Wean to SpO₂ 88-95% |
100% → Wean to SpO₂ 88-92% |
|
PEEP |
5 cmH₂O |
8-15 cmH₂O |
5-10 cmH₂O |
|
I:E Ratio |
1:2 – 1:3 |
1:1 – 1:2 |
1:3 – 1:4 |
|
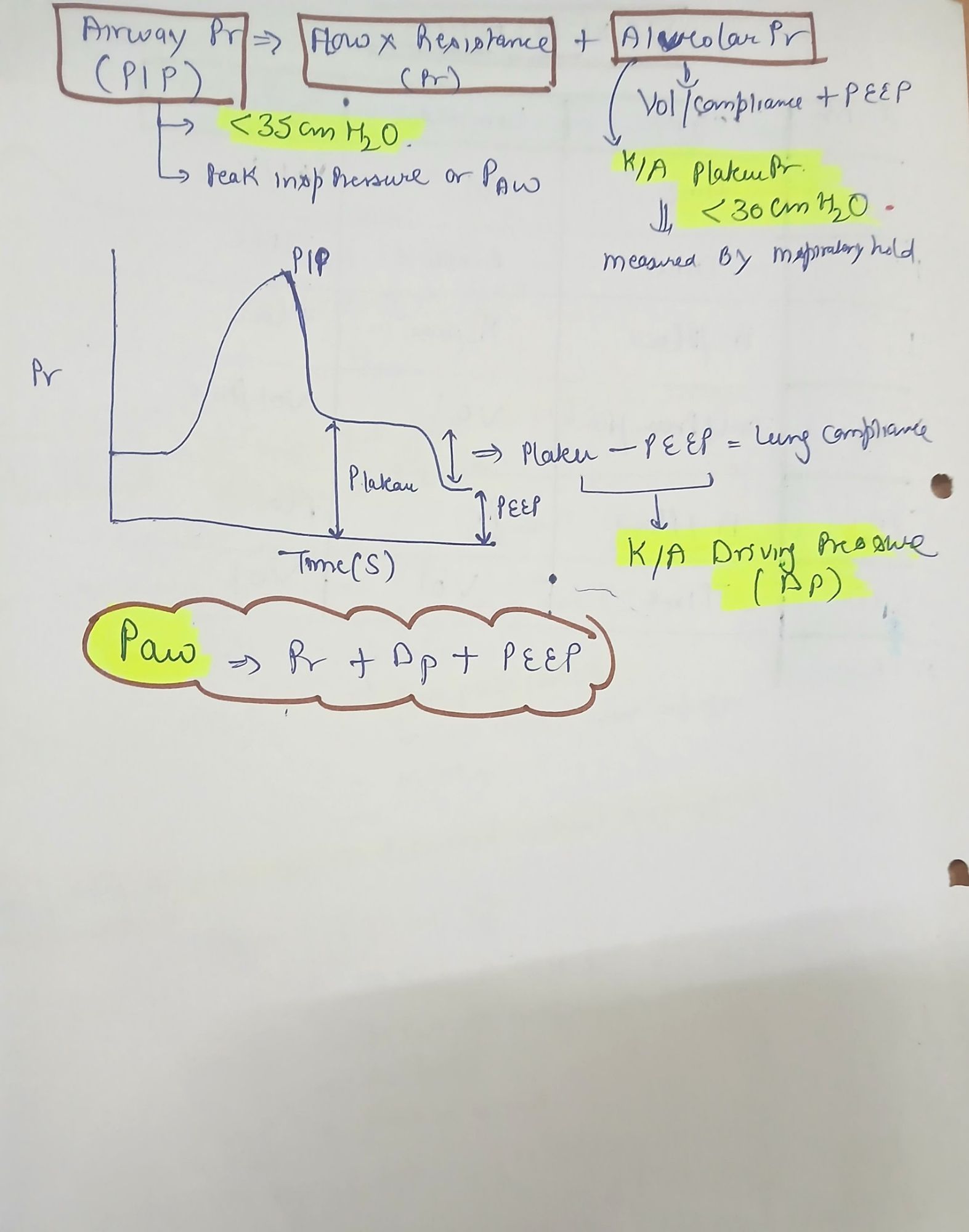
Plateau Pressure (Pplat) |
<30 cmH₂O |
<28 cmH₂O |
<30 cmH₂O |
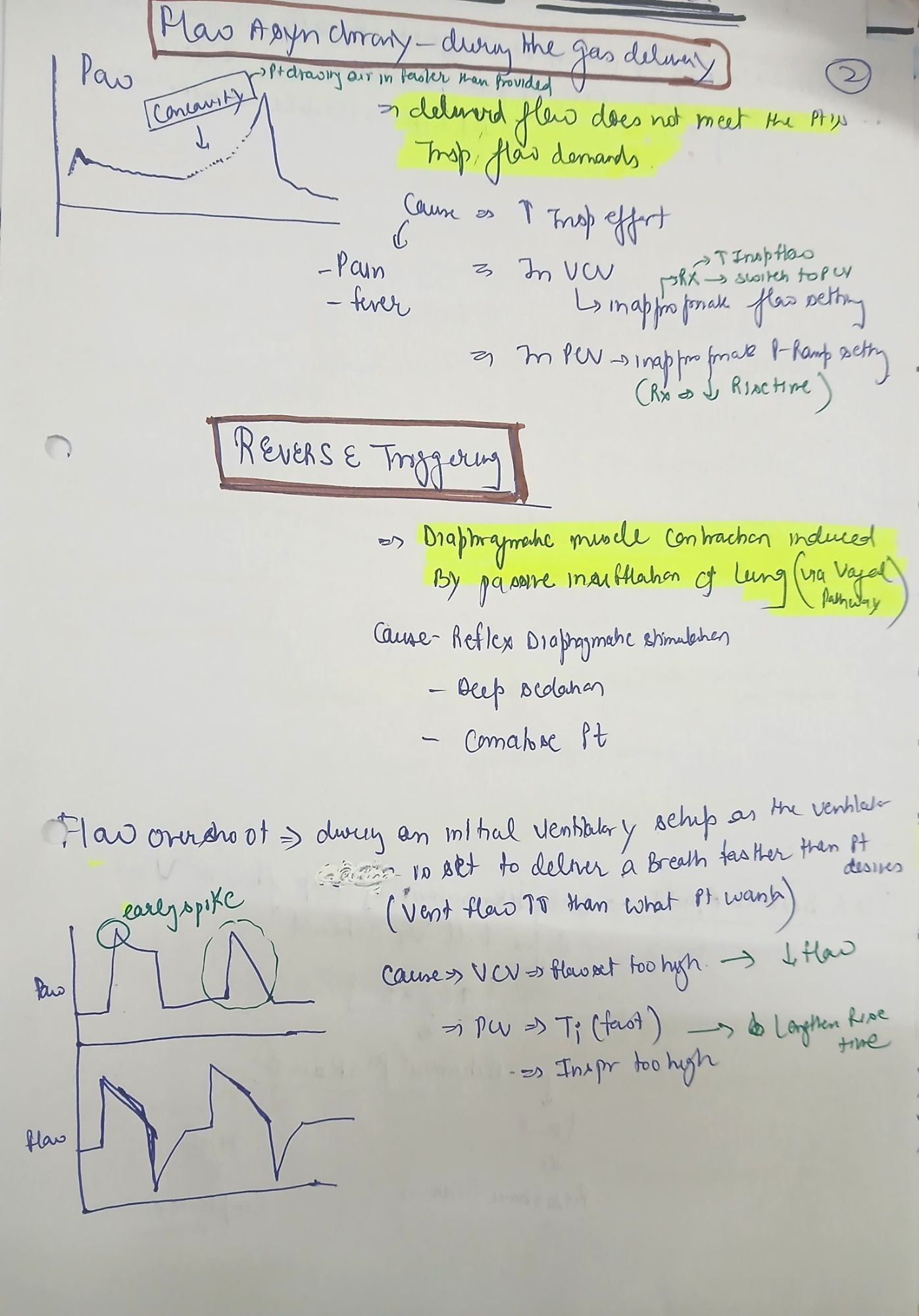
III. Ventilator Asynchrony
A. Types of Patient-Ventilator Asynchrony
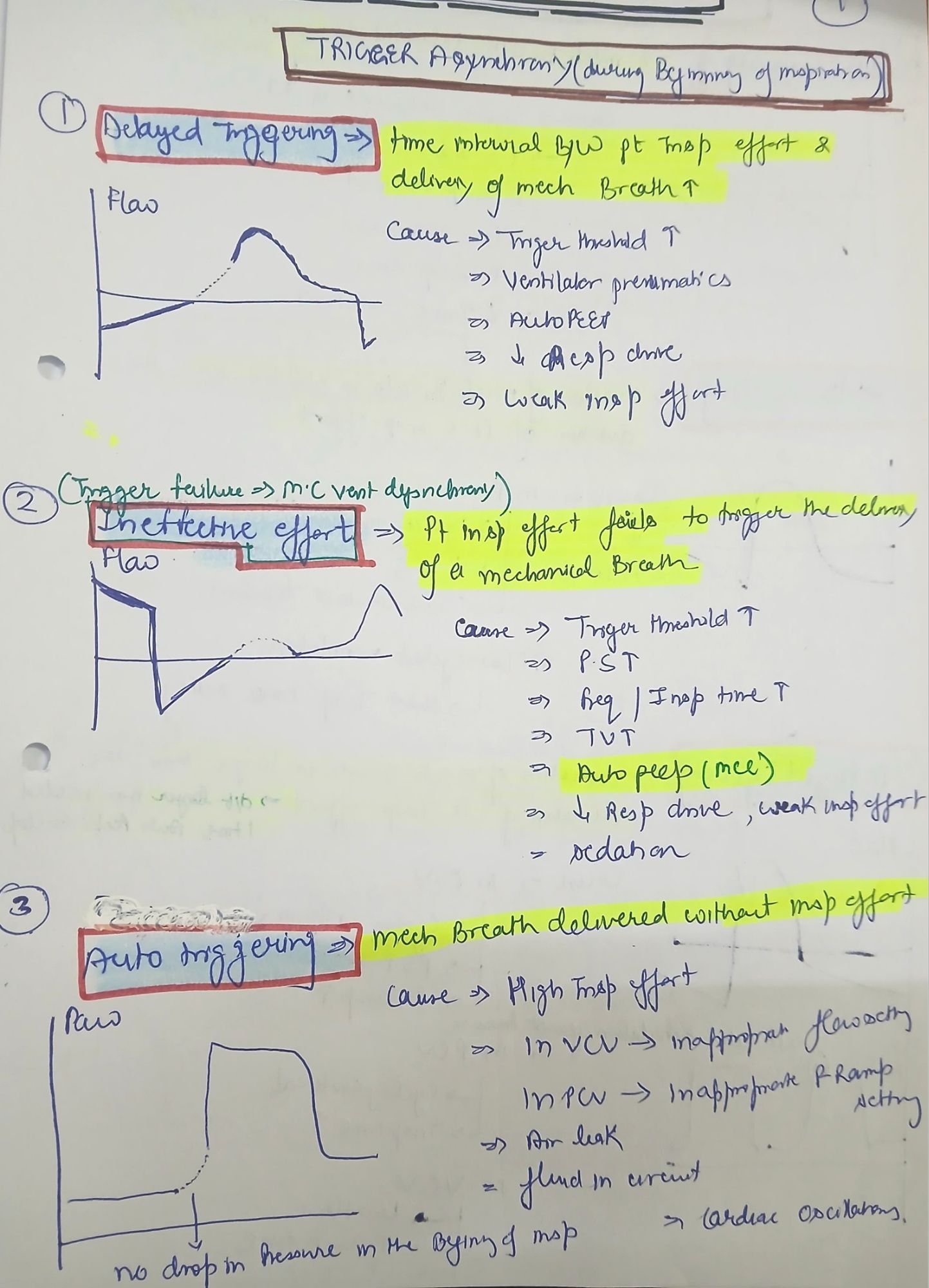
1. Trigger Asynchrony
• Cause: Auto-PEEP, weak respiratory muscles.
• Management: Adjust trigger sensitivity, reduce PEEP.
2. Flow Asynchrony
• Cause: Fixed inspiratory flow in volume-controlled modes.
• Management: Increase inspiratory flow, switch to pressure-controlled mode.
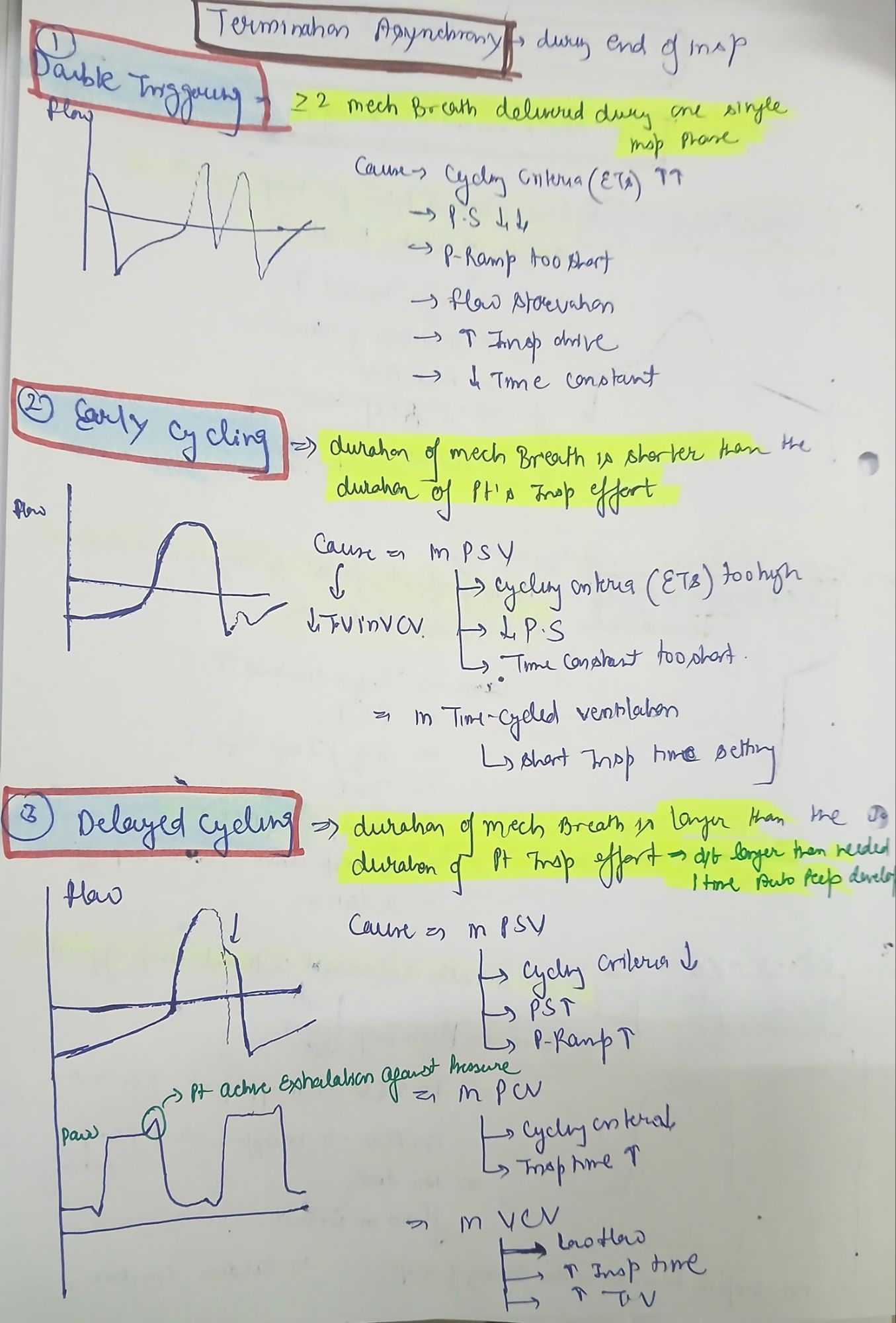
3. Cycle Asynchrony
• Cause: Mismatch between inspiratory time and patient effort.
• Management: Adjust inspiratory time settings.
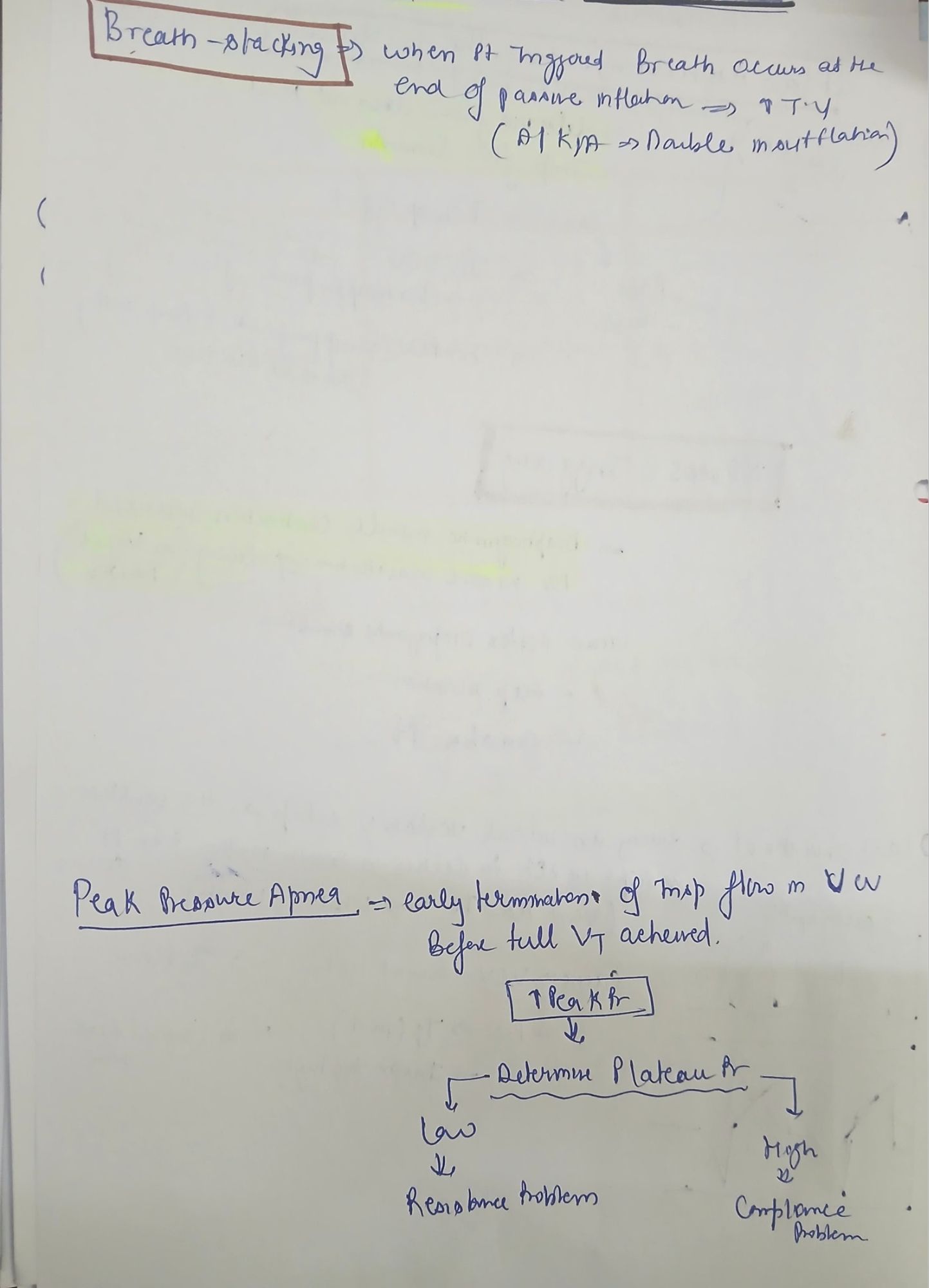
4. Double Triggering
• Cause: Low tidal volume settings.
• Management: Increase tidal volume or inspiratory time.
5. Auto-PEEP (Intrinsic PEEP)
• Cause: Incomplete expiration in obstructive lung disease.
• Management: Increase expiratory time, reduce tidal volume and respiratory rate.
IV. Practical Considerations in Ventilator Management
A. Ventilator-Associated Lung Injury (VILI)
• Barotrauma: High airway pressures (PIP > 35 cmH₂O).
• Volutrauma: High tidal volumes causing alveolar overdistension.
• Atelectrauma: Repeated alveolar collapse due to inadequate PEEP.
• Biotrauma: Inflammatory mediator release due to ventilator stress.
B. ARDSNet Protocol for Lung-Protective Ventilation
• Tidal volume: 4-6 mL/kg IBW
• Plateau pressure: <30 cmH₂O
• PEEP: 8-15 cmH₂O
• Prone positioning if PaO₂/FiO₂ < 150 mmHg
C. Ventilator Weaning
• Readiness criteria:
• Spontaneous breathing trial (SBT) success.
• RSBI (Rapid Shallow Breathing Index) < 105 breaths/min/L.
• FiO₂ < 40%, PEEP ≤ 5 cmH₂O.