Abdominal Distension in the ICU
DEFINITION
Abdominal distension refers to an abnormal increase in abdominal girth or tension, either:
- Visible (inspection)
- Palpable (tense abdomen)
- Measured (serial abdominal girth or rising intra-abdominal pressure)
It may be:
- Acute or chronic
- Localized or generalized
- Painful or painless
- Associated with organ dysfunction
Key ICU Principle
Any new or progressive abdominal distension in a critically ill patient must be assumed pathological until proven otherwise.
PATHOPHYSIOLOGICAL BASIS
From a critical care standpoint, abdominal distension results from one or more of the following fundamental mechanisms:
1. Intraluminal Accumulation
- Gas
- Fluid
- Feces
2. Extraluminal Fluid Accumulation
- Ascites
- Hemoperitoneum
- Pus (peritonitis)
3. Visceral Edema
- Bowel wall edema
- Mesenteric congestion
4. Mass Effect
- Tumors
- Organomegaly
- Cysts
5. Raised Intra-abdominal Pressure (IAP)
- Leading to abdominal compartment syndrome
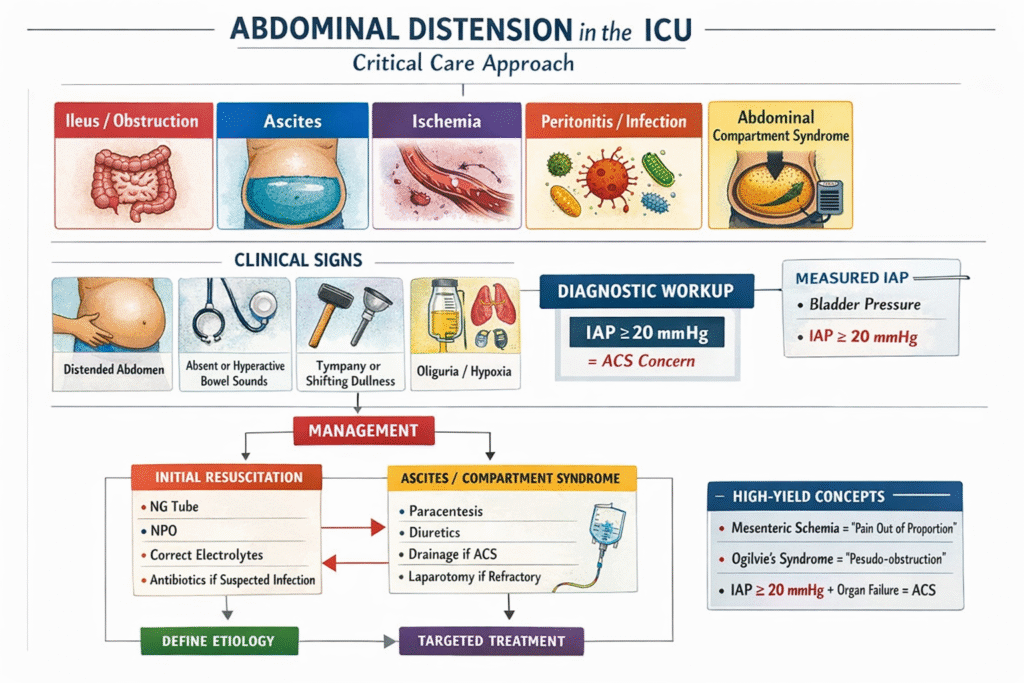
ICU-SPECIFIC ETIOLOGICAL CLASSIFICATION
A. Gastrointestinal Causes
1. Paralytic (Adynamic) Ileus
- Most common cause in ICU
- Functional inhibition of peristalsis
Common ICU Triggers
- Sepsis and septic shock
- Electrolyte disturbances (↓ K⁺, ↓ Mg²⁺)
- Opioids, sedatives, anticholinergics
- Postoperative state
- Severe trauma
- Mechanical ventilation with high PEEP
Clinical Clues
- Uniform abdominal distension
- Absent or hypoactive bowel sounds
- Minimal pain
- No transition point on imaging
2. Mechanical Intestinal Obstruction
- Small bowel obstruction (SBO)
- Large bowel obstruction (LBO)
Etiologies
- Adhesions
- Hernia
- Volvulus (sigmoid, cecal)
- Malignancy
- Fecal impaction
Key Differentiation from Ileus
Feature | Ileus | Mechanical Obstruction |
Pain | Mild | Colicky |
Bowel sounds | Absent | Hyperactive (early) |
Imaging | Diffuse dilation | Transition point |
Gas in rectum | Present | Often absent |
3. Acute Colonic Pseudo-obstruction (Ogilvie’s Syndrome)
- Functional colonic dilation without mechanical blockage
- Common in:
- ICU patients
- Trauma
- Post-operative states
- Severe sepsis
Critical Risk
- Cecal diameter > 12 cm → perforation risk
4. Toxic Megacolon
- Fulminant colitis with systemic toxicity
Causes
- Clostridioides difficile infection
- Ulcerative colitis
- Ischemic colitis
Diagnostic Criteria (Harrison-Style)
- Colonic dilation > 6 cm plus
- Fever, tachycardia, leukocytosis, anemia, hypotension, AMS
B. Hepatology & Portal Hypertension
Massive Ascites
- Cirrhosis (most common)
- Acute liver failure
- Budd–Chiari syndrome
- Malignancy
ICU Relevance
- Respiratory compromise
- Reduced venous return
- Risk of spontaneous bacterial peritonitis (SBP)
- Precipitation of abdominal compartment syndrome
C. Vascular & Ischemic Causes
Acute Mesenteric Ischemia
- SMA embolism or thrombosis
- Non-occlusive mesenteric ischemia (NOMI)
Hallmark
Severe abdominal distension and pain disproportionate to physical findings
Often missed in ICU due to sedation.
D. Infectious Causes
- Secondary peritonitis
- Intra-abdominal abscess
- Tubercular peritonitis (important in India)
- Severe pancreatitis with third-spacing
E. Metabolic & Systemic Causes
- Severe hypoalbuminemia
- Capillary leak syndrome
- Massive fluid resuscitation
- Renal failure with volume overload
F. Iatrogenic & ICU-Related Causes
- Enteral feeding intolerance
- Aerophagia during NIV
- Excessive fluid resuscitation
- High PEEP ventilation
- Post-surgical bowel edema
ABDOMINAL COMPARTMENT SYNDROME (ACS)
Definition
- Sustained IAP ≥ 20 mmHg with new organ dysfunction
Causes
- Massive ascites
- Bowel edema
- Hemoperitoneum
- Retroperitoneal hematoma
- Severe pancreatitis
Physiological Consequences
- ↓ Venous return → ↓ Cardiac output
- ↑ Airway pressures → Hypoxemia
- ↓ Renal perfusion → Oliguria
- ↑ ICP via reduced venous drainage
CLINICAL ASSESSMENT IN ICU
1. Inspection
- Symmetry
- Tense or shiny abdomen
- Dilated veins
- Surgical scars
2. Palpation
- Tenderness (localized vs diffuse)
- Guarding / rigidity
- Organomegaly
- Ascitic thrill
3. Percussion
- Tympany → gas
- Shifting dullness → ascites
4. Auscultation
- Absent sounds → ileus
- High-pitched → obstruction
MONITORING & INVESTIGATIONS
Laboratory
- Electrolytes (K⁺, Mg²⁺)
- Lactate (ischemia)
- LFTs
- ABG (metabolic acidosis)
- Inflammatory markers
Radiology
Bedside Ultrasound
- Ascites
- Dilated bowel loops
- Free fluid
- Bladder volume
X-ray Abdomen
- Air-fluid levels
- Colonic dilation
- Coffee-bean sign (volvulus)
CT Abdomen (Gold Standard)
- Transition point
- Ischemia
- Pneumatosis intestinalis
- Portal venous gas
- Perforation
Intra-abdominal Pressure Monitoring
- Via bladder pressure
- Essential in:
- Severe distension
- Oliguria
- Rising ventilatory pressures
MANAGEMENT PRINCIPLES (ICU-ORIENTED)
1. Immediate Stabilization
- ABC approach
- Nasogastric decompression
- Nil per oral (NPO)
- Correct electrolytes
2. Treat the Underlying Cause
Etiology | Specific Management |
Ileus | Stop offending drugs, mobilization, electrolyte correction |
SBO/LBO | NG tube, surgery consult |
Ascites | Therapeutic paracentesis + albumin |
Ogilvie’s | Neostigmine / colonoscopic decompression |
ACS | Decompression (medical → surgical) |
Ischemia | Urgent revascularization / surgery |
3. Ventilatory Adjustments
- Reduce PEEP if possible
- Monitor plateau pressures
- Consider abdominal decompression before escalating ventilation
4. Nutrition Strategy
- Hold feeds in severe distension
- Prefer post-pyloric feeding
- Avoid overfeeding
PROGNOSTIC IMPLICATIONS
- Persistent distension → ↑ mortality
- Associated with:
- Longer ICU stay
- Ventilator dependence
- Renal failure
- Sepsis

