COAGULOPATHY IN LIVER DISEASE
1. INTRODUCTION
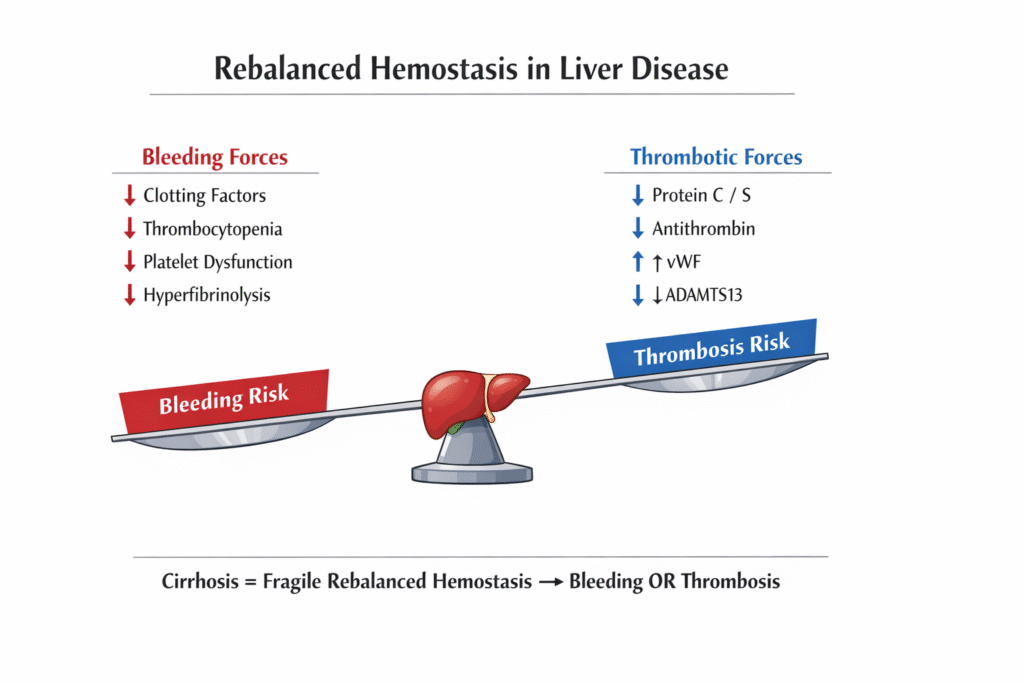
Coagulopathy in liver disease is complex, dynamic, and paradoxical. Unlike classical teaching that cirrhosis causes a “bleeding diathesis,” modern understanding recognizes a state of rebalanced hemostasis, where pro-coagulant and anti-coagulant forces are simultaneously reduced, resulting in fragile equilibrium that can tip toward bleeding or thrombosis.
2. PHYSIOLOGICAL ROLE OF THE LIVER IN HEMOSTASIS
The liver is central to all three components of hemostasis:
A. Coagulation Factors (Pro-coagulant)
Synthesized by hepatocytes:
- Fibrinogen (Factor I)
- Factors II (Prothrombin), V, VII, IX, X, XI
- Factor XIII
- Vitamin K–dependent factors: II, VII, IX, X
B. Natural Anticoagulants
Also synthesized by the liver:
- Protein C
- Protein S
- Antithrombin III
C. Fibrinolytic System
- Plasminogen
- α2-antiplasmin
- Clearance of tPA
D. Platelet Regulation
- Thrombopoietin (TPO) synthesis
- Clearance of activated clotting factors
👉 Thus, liver failure affects clot formation, inhibition, and clot breakdown simultaneously.
3. PATHOPHYSIOLOGY OF COAGULOPATHY IN LIVER DISEASE
A. Reduced Synthesis of Coagulation Factors
- ↓ Factors II, V, VII, IX, X, XI
- Factor VII has the shortest half-life → PT prolongs early
B. Reduced Natural Anticoagulants
- ↓ Protein C, Protein S, Antithrombin III
- Creates pro-thrombotic tendency
C. Thrombocytopenia (Multifactorial)
- Splenic sequestration (portal hypertension)
- ↓ Thrombopoietin synthesis
- Bone marrow suppression (alcohol, sepsis)
- Immune-mediated platelet destruction
D. Platelet Dysfunction
- Impaired adhesion and aggregation
- Altered von Willebrand factor (vWF) interaction
E. Fibrinolytic Abnormalities
- ↓ Clearance of tPA → hyperfibrinolysis
- ↓ Plasminogen
- Net effect varies with disease stage
F. Endothelial Dysfunction
- ↑ vWF
- ↓ ADAMTS13
- Promotes platelet adhesion despite thrombocytopenia
4. REBALANCED HEMOSTASIS – THE MODERN CONCEPT
In chronic liver disease:
|
Pro-Bleeding Forces |
Pro-Thrombotic Forces |
|
↓ Clotting factors |
↓ Natural anticoagulants |
|
Thrombocytopenia |
↑ vWF |
|
Platelet dysfunction |
↓ ADAMTS13 |
|
Hyperfibrinolysis |
Endothelial activation |
👉 Net result:
A new balance that is:
- Unstable
- Easily tipped by infection, AKI, procedures, GI bleed
Here PT/INR reflects only pro-coagulant deficiency, NOT bleeding risk
5. LABORATORY ABNORMALITIES IN LIVER COAGULOPATHY
A. Conventional Tests (Limited Value)
|
Test |
Finding |
Limitation |
|
PT / INR |
Prolonged |
Ignores anticoagulant deficiency |
|
aPTT |
Prolonged |
Poor bleeding predictor |
|
Platelet count |
Low |
Does not reflect function |
|
Fibrinogen |
Normal / ↓ |
Acute phase reactant |
—> INR was designed for warfarin monitoring — NOT cirrhosis
B. Global Coagulation Tests (Preferred in ICU)
Thromboelastography (TEG) / ROTEM
Assesses:
- Clot initiation
- Clot strength
- Fibrinolysis
Advantages:
- Bedside
- Dynamic
- Guides targeted transfusion
6. BLEEDING MANIFESTATIONS
A. Common Bleeding Sites
- Variceal bleeding (portal hypertension – NOT coagulopathy)
- Mucosal bleeding
- Procedure-related bleeding
- Intracranial hemorrhage (rare)
B. Important Concept
– Most GI bleeding in cirrhosis is portal hypertensive, not due to INR elevation
7. THROMBOTIC MANIFESTATIONS (UNDER-RECOGNIZED)
Despite abnormal INR, cirrhotic patients are prone to:
- Portal vein thrombosis
- Deep vein thrombosis
- Pulmonary embolism
- Hepatic artery thrombosis (post-transplant)
👉 Elevated INR does NOT protect against thrombosis
8. COAGULOPATHY IN ACUTE LIVER FAILURE (ALF)
|
Feature |
Chronic Liver Disease |
Acute Liver Failure |
|
INR |
Mild–moderate ↑ |
Markedly ↑ |
|
Platelets |
↓ |
Normal / ↓ |
|
Fibrinogen |
Normal / ↑ |
↓ |
|
DIC-like state |
Rare |
Common |
|
Bleeding risk |
Low–moderate |
High |
ALF resembles consumptive coagulopathy + hyperfibrinolysis
9. MANAGEMENT PRINCIPLES (CRITICAL CARE FOCUS)
A. Do NOT Correct Numbers Prophylactically
- No routine FFP for elevated INR
- No platelet transfusion unless bleeding/procedure planned
B. Indications for Correction
|
Situation |
Target |
|
Active bleeding |
Treat clinically |
|
High-risk procedure |
Platelets >50,000 |
|
Neurosurgery |
Platelets >100,000 |
|
Fibrinogen |
>150 mg/dL |
C. Blood Product Use (Targeted)
|
Product |
Indication |
|
Platelets |
<50k + bleeding |
|
Cryoprecipitate |
Low fibrinogen |
|
FFP |
Massive bleeding |
|
PCC |
Life-threatening bleed |
|
Tranexamic acid |
Proven hyperfibrinolysis |
>—TEG-guided transfusion reduces unnecessary blood use
D. Vitamin K
- Useful only in cholestasis, malnutrition
- Ineffective in synthetic failure
E. Anticoagulation in Cirrhosis
- Safe if indicated (DVT, PVT)
- Requires careful monitoring
- INR unreliable → use clinical judgment
10. COAGULOPATHY VS DIC
|
Feature |
Liver Disease |
DIC |
|
Factor VIII |
Normal / ↑ |
↓ |
|
Fibrinogen |
Normal / ↓ |
↓ |
|
Platelets |
Mild ↓ |
Marked ↓ |
|
D-dimer |
Mild ↑ |
Markedly ↑ |

