🔹 Definition
Acute pancreatitis is an acute inflammatory process of the pancreas with possible involvement of peripancreatic tissues and remote organ systems.
🔬 Revised Atlanta Criteria (2012) – Diagnosis requires ≥2 of:
- Abdominal pain consistent with pancreatitis (epigastric, radiating to back)
- Serum lipase or amylase >3× upper normal limit
- Imaging findings (CT/MRI/USG) consistent with pancreatitis
📊 Classification
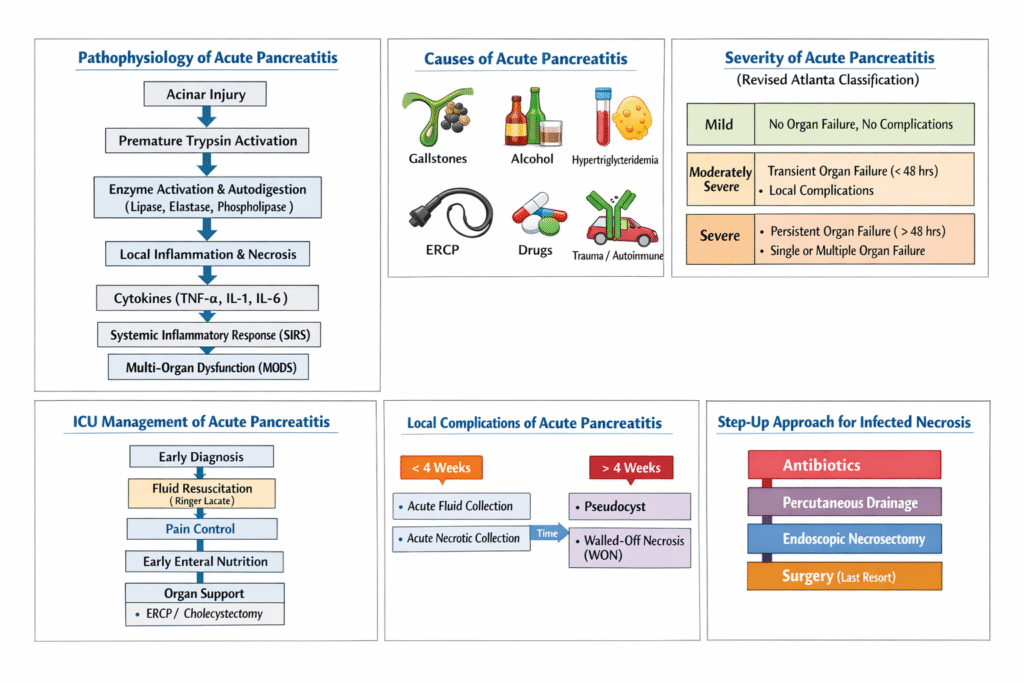
Type | Features |
Mild | No organ failure, no local or systemic complications |
Moderately severe | Transient organ failure (<48h) or local/systemic complications |
Severe | Persistent organ failure (>48h), single or multiple |
🔍 Pathophysiology
- Acinar cell injury → inappropriate trypsinogen activation → autodigestion.
- Release of pro-inflammatory mediators → SIRS, ↑ vascular permeability, third spacing.
- In severe AP: multiorgan dysfunction, local necrosis, infection.
Etiologies: “I GET SMASHED”
- Idiopathic
- Gallstones (40–70%)
- Ethanol (25–35%)
- Trauma
- Steroids
- Mumps/malignancy
- Autoimmune
- Scorpion sting
- Hyperlipidemia/hypercalcemia
- ERCP
- Drugs (thiazides, azathioprine, valproate)
🧪 Severity Scoring Systems
- BISAP (Bedside Index of Severity in Acute Pancreatitis): BUN >25, impaired mental status, SIRS, age >60, pleural effusion
- APACHE II
- CT Severity Index (Balthazar)
Persistent organ failure = best single predictor of mortality.
Management Principles: Logic Behind Each Intervention
1. Fluid Resuscitation
Why: Prevent/treat third-space losses, reduce hypoperfusion-related necrosis.
Mechanism:
- Pancreatic inflammation → SIRS → ↑ capillary leak → intravascular depletion
- Aggressive fluids = ↓ hypoperfusion = ↓ necrosis & mortality
Preferred Fluid:
- Ringer’s lactate > NS (less hyperchloremic acidosis, anti-inflammatory effect)
Dosing:
- Initial bolus: 20 mL/kg over 1 hour if hypotensive
- Maintenance: 3–5 mL/kg/hr (adjust per response: HR, MAP, UO, Hct, lactate)
Goal-directed monitoring:
- UO > 0.5 mL/kg/h
- Hct target: 35–44%
- Avoid fluid overload → ↑ risk of IAH/ARDS
2. Analgesia
Why: Severe visceral pain worsens stress response, respiratory mechanics.
Drugs:
- IV opioids preferred (e.g., fentanyl, hydromorphone)
- Fentanyl
- Avoid morphine in biliary pancreatitis (sphincter of Oddi spasm concern — theoretical)
Logic: Opioids are effective, safe with renal/hepatic adjustment. Consider PCA or continuous infusion.
3. Antibiotics
When to Use:
- Only if infection is suspected/confirmed (e.g., infected necrosis, cholangitis, sepsis)
- Not for prophylaxis in necrotizing AP (RCTs show no mortality benefit)
Empiric Drugs for Infected Necrosis:
- Imipenem (good pancreatic penetration)
- Meropenem, Pip-Tazo, or Cefepime + Metronidazole
Fungal coverage only if patient has prolonged antibiotics, central line, or TPN.
4. Nutrition
Why: Reduces gut barrier dysfunction, bacterial translocation.
Mechanism: Early enteral nutrition maintains gut mucosa, reduces systemic inflammation.
Approach:
- Start enteral feeds within 24–72 hrs, even in severe AP.
- NG =NJ unless severe ileus or high aspiration risk.
- If enteral fails: switch to TPN after 5–7 days.
Formulation: Polymeric or elemental feeds; low-fat in chylous ascites.
5. Management of Necrosis & Collections
Types:
- Acute peripancreatic fluid collection (APFC)
- Pseudocyst (matured >4 weeks, no necrosis)
- Acute necrotic collection (ANC)
- Walled-off necrosis (WON): encapsulated necrosis ≥4 weeks
Intervention:
- Only if infected or symptomatic (pain, obstruction)
- Step-up approach:
- 1st: Antibiotics
- 2nd: Percutaneous drainage / endoscopic transluminal drainage
- 3rd: Video-assisted retroperitoneal debridement (VARD) or surgical necrosectomy
6. ERCP in Gallstone Pancreatitis
When:
- Cholangitis present → urgent ERCP
- Biliary obstruction + high bilirubin → early ERCP (<72 hrs)
- No routine ERCP unless confirmed bile duct obstruction
7. Management of Organ Failure / Complications
Complication | Management |
Hypoxia / ARDS | Low TV ventilation, prone if needed |
AKI | Volume optimization, RRT if refractory |
Shock | Vasopressors (norepinephrine 0.05–0.5 mcg/kg/min) |
IAH / ACS | Monitor bladder pressure, consider decompression |

