ASCITES
1. Definition
Ascites is the pathological accumulation of free fluid in the peritoneal cavity, most commonly due to portal hypertension secondary to cirrhosis.
- Clinically detectable when fluid ≥ 1.5–2 L
- Most common complication of decompensated cirrhosis
2. Epidemiology
- ~60% of patients with compensated cirrhosis develop ascites within 10 years
- Once ascites develops → 5-year survival ≈ 50%
- Major cause of hospital admission in liver disease
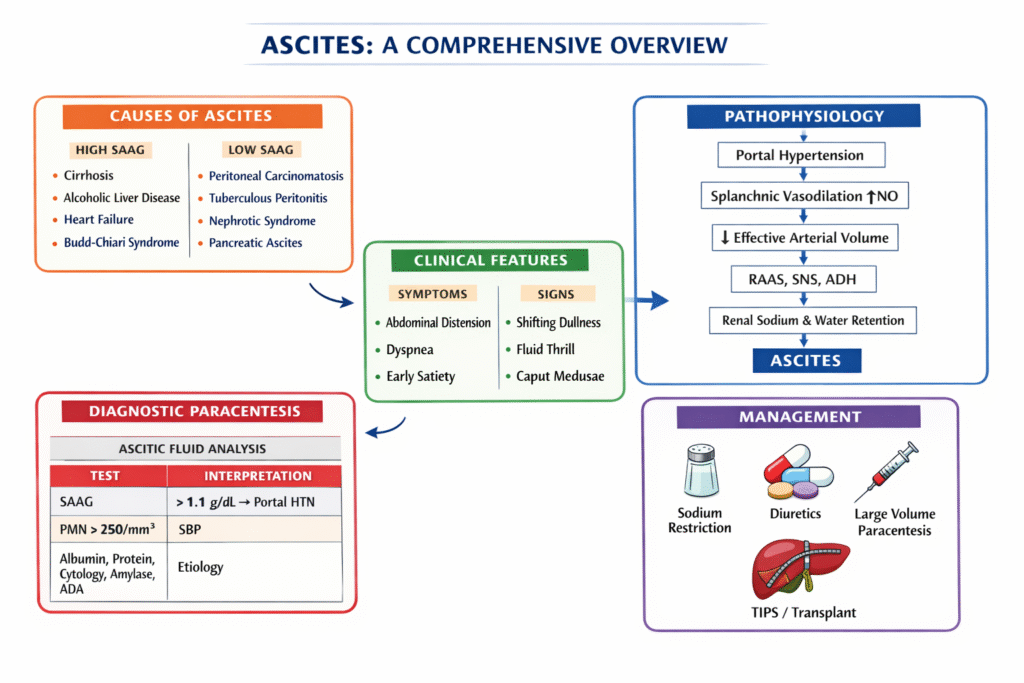
3. Etiology of Ascites
A. Portal Hypertension–Related (High SAAG)
- Cirrhosis (most common)
- Alcoholic liver disease
- Viral hepatitis (HBV, HCV)
- NASH
- Budd–Chiari syndrome
- Cardiac cirrhosis / constrictive pericarditis
B. Non–Portal Hypertension (Low SAAG)
- Peritoneal carcinomatosis
- Tuberculous peritonitis
- Pancreatic ascites
- Nephrotic syndrome
- Serositis (SLE)
4. Pathophysiology of Ascites
Central Concept: Portal Hypertension + Splanchnic Vasodilation
Stepwise Mechanism:
- Portal hypertension → ↑ sinusoidal pressure
- ↑ Nitric oxide → splanchnic vasodilation
- ↓ Effective arterial blood volume (arterial underfilling)
- Activation of:
- RAAS
- Sympathetic nervous system
- ADH
- Renal sodium and water retention
- Fluid transudation into peritoneal cavity
Key Hypotheses (Harrison):
- Peripheral arterial vasodilation hypothesis (most accepted)
- Overflow hypothesis (obsolete)
5. Clinical Features
Symptoms
- Progressive abdominal distension
- Weight gain
- Dyspnea (↑ intra-abdominal pressure)
- Early satiety
- Lower limb edema
Signs
- Shifting dullness
- Fluid thrill
- Umbilical hernia
- Caput medusae
- Signs of chronic liver disease
6. Grading of Ascites (International Ascites Club)
Grade | Description |
Grade 1 | Mild, detectable only by ultrasound |
Grade 2 | Moderate, symmetrical distension |
Grade 3 | Large / tense ascites |
7. Diagnostic Evaluation
A. Diagnostic Paracentesis (MANDATORY)
All new-onset ascites → diagnostic tap
Ascitic Fluid Analysis
Parameter | Interpretation |
Cell count | PMN ≥ 250/mm³ → SBP |
Total protein | <2.5 g/dL → cirrhotic |
Albumin | For SAAG |
Culture | SBP |
ADA | TB ascites |
Amylase | Pancreatic ascites |
Cytology | Malignancy |
8. SAAG (Serum–Ascites Albumin Gradient)
Formula:
SAAG = Serum albumin – Ascitic fluid albumin
Interpretation:
- SAAG ≥ 1.1 g/dL → Portal hypertension
- SAAG < 1.1 g/dL → Non-portal causes
SAAG | Cause |
High | Cirrhosis, cardiac ascites, Budd–Chiari |
Low | TB, malignancy, pancreatitis |
SAAG is superior to total protein for etiological diagnosis
9. Management of Ascites
A. General Measures
- Treat underlying cause
- Avoid NSAIDs
- Avoid ACE-I / ARBs in advanced cirrhosis
- Alcohol abstinence
B. Sodium Restriction
- <2 g/day (≈ 88 mmol/day)
- Water restriction only if Na <125 mEq/L
C. Diuretics-oral (First-line)
Drug | Dose |
Spironolactone | 100 mg/day |
Furosemide | 40 mg/day |
Maintain 100:40 ratio
Max doses:
- Spironolactone 400 mg/day
- Furosemide 160 mg/day
Target weight loss:
- With edema: ≤1 kg/day
- Without edema: ≤0.5 kg/day
D. Large Volume Paracentesis (LVP)
- For tense / refractory ascites
- Remove >5 L safely
Albumin replacement:
- 6–8 g albumin per liter removed
Prevents paracentesis-induced circulatory dysfunction
10. Refractory Ascites
Definition
Ascites that cannot be mobilized or recurs rapidly despite:
- Sodium restriction
- Maximal diuretics
Management
- Repeated LVP + albumin
- TIPS (Transjugular Intrahepatic Portosystemic Shunt)
- Liver transplantation (definitive)
11. Complications of Ascites
A. Spontaneous Bacterial Peritonitis (SBP)
- PMN ≥250/mm³
- Common organisms: E. coli, Klebsiella
- Treat: 3rd gen cephalosporins
B. Hepatorenal Syndrome (HRS)
- Functional renal failure
- Triggered by SBP, LVP without albumin
C. Others
- Umbilical hernia rupture
- Hyponatremia
- Respiratory compromise
12. Special Types of Ascites
A. Cardiac Ascites
- High SAAG, high protein
- Treat heart failure
B. Chylous Ascites
- Milky fluid
- Triglycerides >200 mg/dL
- Causes: lymphoma, TB
C. Pancreatic Ascites
- Very high amylase
- Low SAAG
13. Prognosis
- Ascites = marker of decompensation
- Median survival after onset ≈ 2–3 years
- Best long-term treatment: liver transplantation

